Clinical
Measuring near lag of accommodation
In this article:
Originally published: December 11, 2015
Updated: December 10, 2020
Assessing accommodative function, such as measuring near lag of accommodation, is a vital component of understanding the myopia profile of your patient. Myopic progression in children and adults can be influenced by binocular vision function. There is a reported association between higher levels of esophoria and accommodative lag at near in myopic children and young adults as compared to emmetropes.1-5 Myopic children and young adults also show insufficient accommodative responses to lens-induced blur,1, 6-8 greater variability in accommodative response9, reduced accommodative facility4, 8 and enhanced accommodative convergence (elevated AC/A ratios) when compared to age matched emmetropes.10-12 There is speculation in the literature regarding accommodative lag prior to onset of myopia - evidence shows higher accommodative lag in progressing myopes, regardless of their starting point of refraction as an emmetrope or myope,4 however other studies do not match this significance.13 Myopia development and progression is multifactorial, though, that it's important to assess all contributory factors - the myopia profile is designed to guide you through this clinical decision making and communication process.
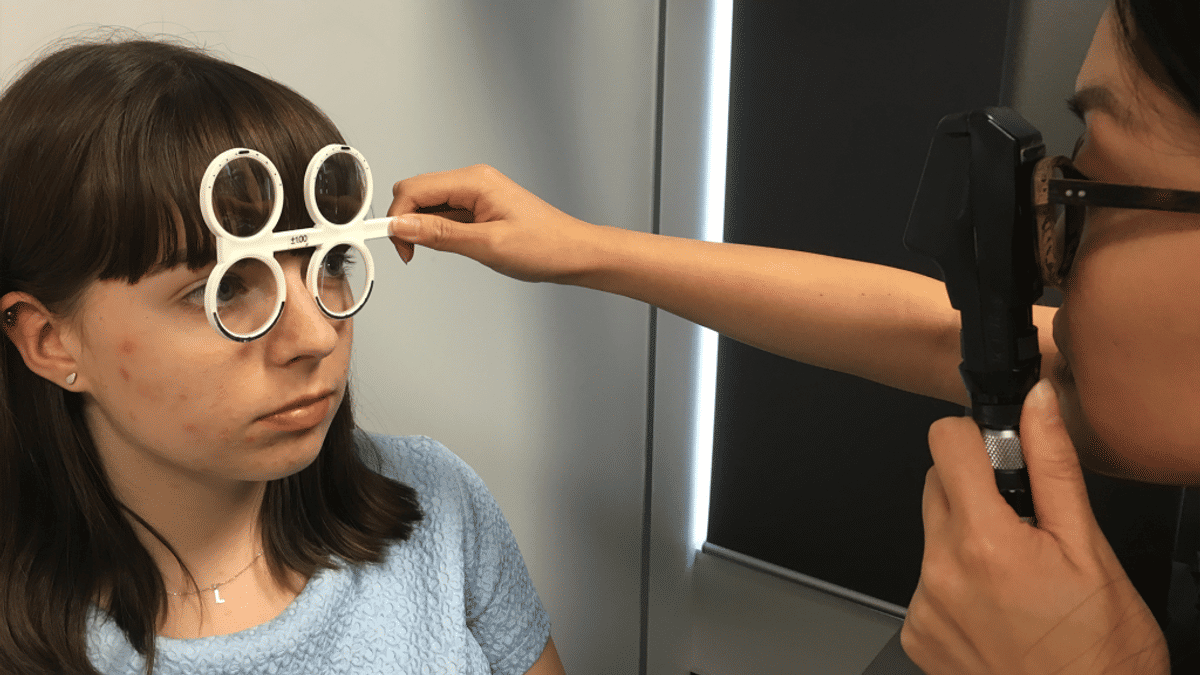
The simplest way to measure accommodative lag is with near retinoscopy. Position yourself 33-40cm away from the patient (2.5-3D accommodative demand), at their near working distance, and have them either look at your nose or a near fixation card attached to your retinoscope. Ensure they have their full distance correction in place. I use ±1.00, ±1.50 and ±2.00 flippers and will start with looking at the reflex without a correcting lens, sweeping quickly along the horizontal and vertical, checking right then left eyes and then repeating. Try the +1.00 flippers first, and if you still see ‘with’ movement, quickly change to +1.50. If the reflex reverses, you’ve got your answer at +1.25. You can combine plus and minus sides of your flippers to get +0.50 or -0.50. Once you’ve got neutralisation or reversal, your last lens is your answer – there’s no correcting calculation required as there is for distance retinoscopy. This technique is termed MEM retinoscopy – alternatively, Nott retinoscopy involves keeping the plane of fixation steady with the examiner moving forwards or backwards to find the neutralised reflex.14
Some of my colleagues use near fixation cards, and this will usually give you a slightly less plus result. There is no universally recommended technique so I'd suggest you get comfortable with one technique, either with or without fixation card, and stick with it to allow easy clinical comparisons. It could be argued that measuring lag with a fixation card is a truer picture of real world function, as it's measuring active accommodation, but conversely measuring with a nose fixation target could see less influence of the testing itself on subconscious accommodative tone. I'm interested in your thoughts on this if you'd like to comment below.
You can also measure accommodative lag with the fused cross-cylinder card in your phoropter. I've found that this can give paradoxical results compared to the free space technique, as active accommodators can get 'confused' by awareness of the big thing in front of their face and demonstrate a lead of accommodation on fused X-cyl where I've already seen a lag on near retinoscopy. A literature search turned up a paper from 1989 which found significantly lower results with fused X-cyl measurement of the near accommodative response compared to MEM or Nott retinoscopy techniques.15 Ultimately I'm interested in assessing the patient's visual function in the closest to normal visual environment, hence I always prefer free space techniques - and not to be forgotten that MEM retinoscopy is also a lot faster!
If you’re lucky enough to have an open field autorefractor, then you’ll be measuring accommodative lag to gold standard. In comparing techniques, one study found good agreement between MEM and Nott retinoscopy results but underestimation of accommodative lag with both compared to open field autorefractor. The authors cited a variety of methodological differences between the techniques as contributing to this result. Interaction between examiner and participant in the retinoscopy techniques, along with the ability of the examiner to observe and measure a stable accommodative response – not possible with autorefraction – could mean different factors of the response are being measured.14
Back in your consulting room: grab your retinoscope and flippers, and give near retinoscopy a try. If you’re waiting for your flippers to arrive then grab a ret rack, quickly change lenses in a trial frame, or use the fused cross-cylinder technique. But I really think you should order some flippers and make your life easier. With some practice you’ll be getting your accommodative lag measurement in under 20 seconds, with this giving you more than enough time to observe the reflex, see if it’s stable and neutralise accurately with your flippers. Normal results are between +0.50 and +1.00, with results higher than this indicating an increased risk for the myopia profile.4, 5, 11, 16, 17
To watch this technique in action, check out our Youtube video on How to measure accommodative lag. You can also watch how to assess accommodative facility on our YouTube channel. If you'd like to reinforce this with text, read more on how to measure accommodative facility, and advice on prescribing for accommodative lag via these links.
NB: You can order flippers in Australia from Cyclopean Designs, either complete or just the flipper frames which you can then have fit at your local lens laboratory.
To delve more into my simplified two-system approach to BV diagnosis and management, you can watch this video entitled Binocular Vision - easier than you think. This one hour lecture includes cases; details easy use of prism correction for vergence disorders; changes to BV in contact lens wear; and why BV matters - for reading and learning in kids, clinical problem solving, and myopia management. You can also download my lecture notes here.
Watch these Myopia Profile YouTube videos on binocular vision techniques:
Read more about accommodation, binocular vision and myopia:
Want to learn more about binocular vision?
Check out my online course Binocular Vision Fundamentals, which starts with my two-system approach to BV assessment and diagnosis. Stepping through understanding of the accommodation and vergence systems, the course then covers clinical tests, diagnostic criteria, prescribing and management. Once this foundation is set, it moves onto clinical communication and the importance of BV in myopia management. Always with a laser sharp focus on the clinical applications.
Included are video examples of assessment techniques and chairside infographic summary downloads to reference in practice.
You can enroll on the first two modules for free, with the full course priced at US$140 if you decide to continue. Reduced course fees by 30% and 50% are available by application for practitioners residing in lower income countries - check out the course page for more information.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
References
- Gwiazda J, Bauer J, Thorn F, Held R. A dynamic relationship between myopia and blur-driven accommodation in school-aged children. Vision Res. 1995;35:1299-1304. (link)
- Nakatsuka C, Hasebe S, Nonaka F, Ohtsuki H. Accommodative lag under habitual seeing conditions: comparison between myopic and emmetropic children. Jap J Ophthalmol. 2005;49:189-194. (link)
- Drobe B, de Saint-André R. The pre-myopic syndrome. Ophthalmic Physiol Opt. 1995;15:375-378. (link)
- Allen PM, O'Leary DJ. Accommodation functions: Co-dependency and relationship to refractive error. Vision Res. 2006;46:491-505. (link)
- Price H, Allen PM, Radhakrishnan H et al. The Cambridge Anti-Myopia Study: Variables Associated with Myopia Progression. Optom Vis Sci. 2013;90:1274-1283. (link)
- Bullimore MA, Gilmartin B, Royston JM. Steady-state accommodation and ocular biometry in late-onset myopia. Documenta Ophthalmologica. Adv Ophthalmol. 1992;80:143-155. (link)
- Abbott ML, Schmid KL, Strang NC. Differences in the accommodation stimulus response curves of adult myopes and emmetropes. Ophthalmic Physiol Opt. 1998;18:13-20. (link)
- Pandian A, Sankaridurg PR, Naduvilath T et al. Accommodative Facility in Eyes with and without Myopia. Invest Ophthalmol Vis Sci. 2006;47:4725-4731. (link)
- Harb E, Thorn F, Troilo D. Characteristics of accommodative behavior during sustained reading in emmetropes and myopes. Vision Res. 2006;46:2581-2592. (link)
- Gwiazda J, Grice K, Thorn F. Response AC/A ratios are elevated in myopic children. Ophthal Physiol Opt. 1999;19:173-179. (link)
- Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optom Vis Sci. 2005;82:273-278. (link)
- Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A Ratio, Age, and Refractive Error in Children. Invest Ophthalmol Vis Sci. 2000;41:2469-2478. (link)
- Rosenfield M, Desai R, Portello JK. Do progressing myopes show reduced accommodative responses? Optom Vis Sci. 2002;79:268-273. (link)
- Correction of Myopia Evaluation Trial 2 Study Group for the Pediatric Eye Disease Investigator Group. Accommodative lag by autorefraction and two dynamic retinoscopy methods. Optom Vis Sci. 2009;86:233-243. (link)
- Locke LC, Somers W. A Comparison Study of Dynamic Retinoscopy Techniques. Optom Vis Sci. 1989;66:540-544. (link)
- Gwiazda JE, Hyman L, Norton TT et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004;45:2143-2151. (link)
- Mutti DO, Mitchell GL, Hayes JR et al (CLEERE Study Group). Accommodative Lag before and after the Onset of Myopia. Invest Ophthalmol Vis Sci. 2006;47:837-846. (link)
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.












