Clinical
Combining the Essilor® Stellest® lens with atropine – Q&A with Dr Bryan Sim
Sponsored by
Childhood myopia, a growing concern globally, poses significant challenges to eyecare professionals (ECPs) and parents alike. As rates of myopia continue to soar, the imperative to explore innovative approaches to manage its progression becomes ever more pressing. In today's clinical practice, atropine eye drops, spectacle lenses with highly aspherical lenslets (HAL), and myopia progression control contact lenses are widely employed to manage and slow the progression of childhood myopia. Among these approaches, combination therapy of atropine eyedrops with HAL spectacle lenses has emerged as a promising strategy.
We talk to Dr Bryan Sim, consultant ophthalmologist with the Myopia Service at the Singapore National Eye Centre (SNEC) about the rationale behind integrating these two modalities, addressing both clinical and practical inquiries essential for understanding their potential synergy in everyday clinical practice with the ultimate aim of reducing childhood myopia progression.
In this article:
What guides your prescribing decisions when it comes to myopia?
Bryan: The main factors that steer our decision on which myopia control modality would best be tailored for the individual patient would be based on:
- Myopia risk progression profile (high risk, marginal, low risk groups), including magnitude of baseline myopic refractive error, axial length (AXL), family history of high myopia, and myopic macular degeneration (MMD) grading
- Patient and parental expectations of childhood control of myopia progression (e.g. acceptance of daily eyedrop administration, full-time wear of spectacles, contact lenses in children)
- Existing ocular conditions e.g. allergic eye disease, epiblepharon with lash corneal touch
- Hobbies and lifestyle preferences e.g. avid sports player, interested in dancing, spectacles-free preference
When it comes to selecting a treatment option, clinical evidence and efficacy of various myopia control treatment modalities are very important. So interventions, not in any order of preference, are:
- Lifestyle modifications: At least 2 hours a day spent outdoors decreases myopia onset in 30%, reduces myopia progression.1,2 Increase light indoors, less intensive near work with regular eye breaks, including minimising screen time (i.e. computers, phones, handheld tablets) would all be part of the lifestyle advice I would recommend.
- Atropine:3-5 Low-dose atropine nightly or twice daily and high dose atropine 3-4 times per week to nightly.
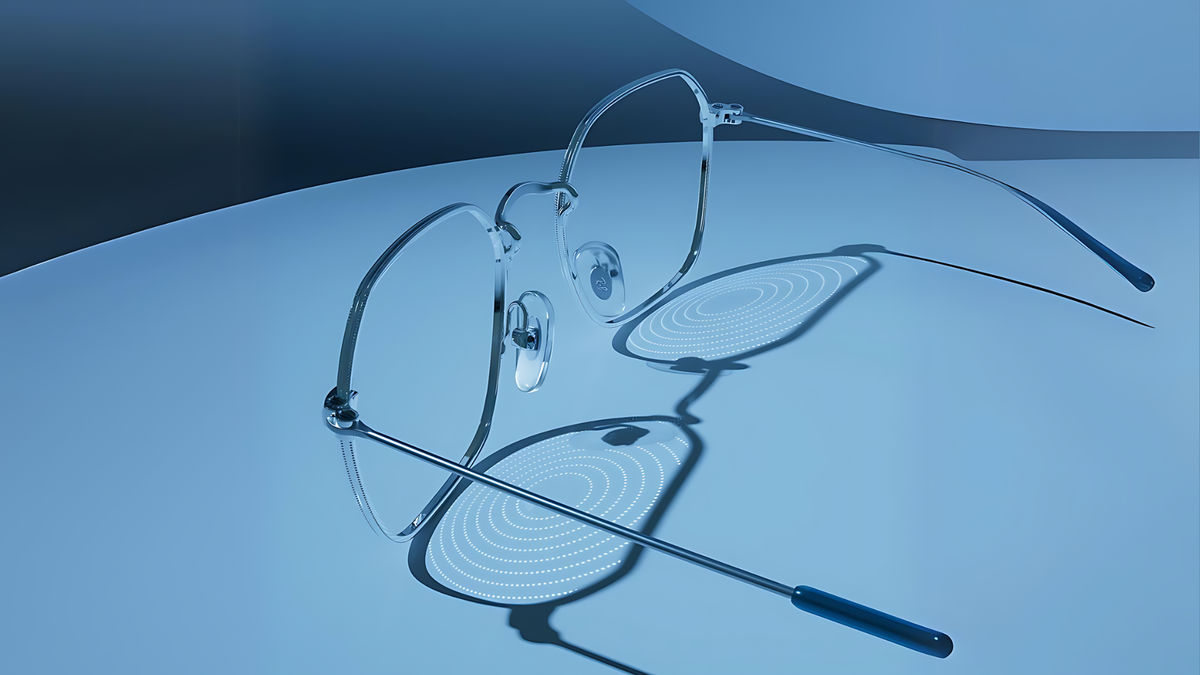
- Myopia control spectacle lenses (e.g. Essilor® Stellest® lenses, which are based on the optical design of spectacle lenses with Highly Aspherical Lenslets or HAL):6-7 full-time wear of spectacle lenses with H.A.L.T. technology can be recommended. The correction range is from plano to – 12.00 D and corrects astigmatism up to 4.00D. For children already wearing spectacles and motivated to wear them full time, it is possible to use them in combination with low-dose atropine in children with high/progressive myopia as a first- or second-line therapy. For children with high myopia out of the correction range, an alternative would be to consider HAL spectacle lenses with single vision contact lenses to correct residual refractive error (if the child and parents are keen and motivated).
- Myopia control contact lenses: soft contact lenses with peripheral defocus, rigid gas permeable (RGP) contact lenses, and orthokeratology.
- Combination therapy: HAL spectacle lenses with atropine drops.
Early intervention is crucial in limiting myopia progression and preventing the development of high myopia later in life. Implementing evidence-based practices, such as lifestyle modifications, optical myopia progression control spectacles, atropine, myopia progression control contact lenses, and combination therapies, forms the foundation of effective management. Strategies should take a holistic approach, offering a comprehensive array of myopia control treatments. Personalized treatment is essential, with each patient’s unique myopia profile—assessed through patient data, progression, and risk-benefit stratification—guiding the choice of the most appropriate myopia control strategy. Children at higher risk for myopia progression typically have a strong family history of parental myopia, a younger age of myopia onset, a higher myopic spherical equivalent (SE) at baseline, or the presence of myopic macular degeneration (MMD) changes.
How has your experience been with combining spectacle lenses with highly aspherical lenslets (HAL spectacle lenses) with atropine?
Bryan: It has been excellent. Combination therapy with HAL spectacle lenses and low-dose atropine is safe and well tolerated amongst children of a wide age range with minimal visual distortion. This is especially true for children who need spectacles to correct their vision or already wearing spectacles and are motivated to wear spectacles full time (at least 12 hours a day).
We conducted a one-year prospective non-randomised controlled observational study to assess the efficacy of adding HAL spectacle lenses to children who are still progressing on low-dose atropine. This is also the first worldwide prospective study combining HAL spectacle lenses and atropine for myopia progression control in Singaporean Asian children. In terms of inclusion criteria, our study involved 50 myopic children aged 6 to 11 years, with myopia ranging from -1.50D to -6.00D and astigmatism of less than -2DC. They were already on atropine 0.01% or 0.025% with good compliance and had shown myopia progression of more than -0.50D in at least one eye over the past 6 months. These children were given HAL spectacle lenses. The key outcome measures including spherical equivalent refraction (SER), cycloplegic autorefraction (CAR) and AXL, were measured at baseline and after 6 and 12 months.
Our study revealed that combination therapy of HAL spectacle lenses with low-dose atropine is more effective in slowing myopia SE and AXL progression than either intervention alone. Further analysis showed:
- A 75% reduction in SE change and 42% reduction in AXL change at 1 year
- Hyperopic shift noted in SE was 28% at 1 year and stability of AXL at 24% at 1 year
- A significant subgroup of patients with sustainable stability in AXL measurement
However, we do acknowledge that:
- 20% still progressed >0.5D over 12 months
- 18% still progressed >0.3mm over 12 months
- 40% progressed >0.15mm over 12 months
Regardless, combination therapy is a promising approach and presents a paradigm shift in our clinical practice. When used in combination with high-dose atropine in children who experience side effects of near blur and glare, using other options such as HAL tinted spectacle lenses, wearing a sunhat or visor outdoors can help overcome the photophobia.
Children should be encouraged to go outdoors to play to delay myopia progression.8 Tinted HAL spectacle lenses provide adequate protection against sun damage and children should be encouraged to wear tinted spectacles, clip on sunglasses, a sunhat or visor outdoors which would motivate them to play outdoors.
What would you recommend or advise practitioners on how and when to combine HAL spectacle lenses with atropine?
Bryan: For practitioners considering how and when to combine HAL spectacle lenses with atropine in managing progressive myopia, it is recommended to consider combination therapy when a child presents with progressive myopia that is not adequately controlled by either optical or pharmacological monotherapy. Specifically, if a child does not respond to atropine eyedrops or myopia progression control glasses/contact lenses alone, they may benefit from the combined use of HAL spectacle lenses and atropine.
HAL spectacle lenses can serve as either a first-line or second-line myopia control therapy in children with high or progressive myopia. For instance, if a child with progressing myopia is already on low-dose atropine nightly (such as 0.01%, 0.025%, 0.05%, or 0.1%) while using single-vision lenses, switching the single vision lenses for HAL spectacle lenses may enhance myopia control efficacy. On the other hand, if myopia continues to progress rapidly despite already being on HAL lenses, one may consider augmenting myopia control with the addition of low-dose atropine eyedrops at night to minimise the side effect profile of near blur and glare in the day or during schooltime.
We generally advise slightly higher dose low-dose atropine (e.g. 0.025%, 0.05%) for younger children less than 9 years old due to their higher-risk myopia progression profile, compared to their older counterparts. Traditionally, we taper atropine drops at 12 years old but with combination of HAL spectacle lenses and atropine, we consider tapering atropine drops earlier at 10 years old.
Children with progressing myopia who are not candidates for myopia progression control contact lenses e.g. children with sensitive/allergic eyes, blepharitis or lid conditions e.g. epiblepharon with lash corneal touch, which places them at higher risk for infective keratitis, may be more suited for combination therapy with HAL spectacle lenses and atropine eyedrops.
Have you found any effect on visual function with combination therapy involving HAL spectacle lenses?
Bryan: Rarely, though anecdotally, some children may experience mild visual distortion in their peripheral vision. However, this visual distortion in a small handful of children is largely transient and children usually adapt to it nicely within a few days. With the added effect of atropine eyedrops, this may cause increased near blur and glare in higher doses of atropine. The glare/photophobia associated with high-dose atropine can be mitigated with the use of HAL spectacle lenses with sun tints (which brings about the added benefit of optical myopia control), clip on sunglasses, a sunhat or visor especially when outdoors.
How do you approach patient education and compliance in myopia management? What were your observations in terms of impact with increased wearing time of HAL spectacle lenses, for example?
Bryan: During counselling on the wide range of childhood myopia control treatment modalities, we would advise the child and parents on the following:
- HAL spectacle lenses can slow myopia by 50-60% (over 2-3 years).6,9 Increased wearing time or full-time wear can result in better myopia control efficacy of up to 67% on average*
- Combination therapy of HAL spectacle lenses with atropine eyedrops works well for children of all ages
- Reinforce full-time HAL spectacle lens wear to achieve optimal myopia control (at least 12 hours/day)
- Children with strabismus on atropine therapy may benefit from combination therapy with HAL spectacle lenses (though the potential risk of deteriorating strabismus control should be advised – under further investigation)
- Follow up process: Reassess spherical equivalent refraction and axial length every 3-6 months initially. Effect is better in the 1st year than in the 2nd year.
- What happens if myopia continues to progress: Try alternate treatment, add low-dose atropine for combination therapy (especially for children less than 7 years old).
- When to stop spectacles: Likely till 13-18 years old or when myopia progression may stabilize. There is currently no evidence of rebound with cessation of HAL spectacle lenses.10 Will need a slow taper of atropine if the patient is on combination therapy.
*Compared to single vision lenses, when worn 12 hours per day, every day for two consecutive years
Do you have case examples to share where you have seen positive results of combination therapy with HAL spectacle lenses and low-dose atropine?
Bryan: In my clinical practice, I have observed significant positive outcomes in patients undergoing combination therapy with HAL spectacle lenses and low-dose atropine. These cases demonstrate the potential for enhanced myopia control, especially in children who do not respond adequately to monotherapy. Here are two case examples that highlight the effectiveness of this approach, illustrating how combining these treatments can result in stabilized refraction and reduced axial elongation, leading to favourable and sustainable outcomes:
Case example A
6-year-old boy presented to the Myopia Centre in Singapore with progressing myopia, despite being on low-dose atropine eyedrops nightly. The child’s mother was not keen to increase the atropine concentration further for concerns of side effects of near blur and glare. After some discussion, the mother opted for an optical intervention: namely, HAL spectacle lenses.
| October 21 | April 22 | November 22 | April 23 | November 23 | |
| Age | 6 | 7 | 8 | 9 | 9 |
| RE AXL | Not obtained | 25.42mm | 25.55mm | 25.48mm | 25.44mm |
| LE AXL | Not obtained | 25.44mm | 25.59mm | 25.59mm | 25.56mm |
| Refraction | Cyclorefraction | Cyclorefraction | Cyclorefraction | Manifest refraction | Cyclorefraction |
| RE Sph | -2.50 | -3.25 | -3.25 | -3.00 | -2.75 |
| LE Sph | -2.75 | -3.25 | -3.75 | -3.75 | -3.75 |
| Treatment and notes | Started atropine 0.01% nightly) | Increased to atropine 0.025% nightly | Combination HAL + Atropine 0.025% nightly | Best corrected visual acuity in RE 6/6-1 and LE 6/6-1 |
As seen from this case illustration, within six months, very good myopia control efficacy with the combination of HAL spectacle lenses and low-dose atropine was achieved. In addition, there was also a small reduction in axial length, which is not very common, and strongly indicates positive patient outcomes. The AXL and SER remained stable over 1 year from starting combination therapy with HAL spectacle lenses showcasing the sustainable effect of combination therapy.
Case example B
6-year-old girl with myopic parents was started on atropine 0.025% nightly in December 2021 due to progressive myopia by a private ophthalmologist. She is an avid book reader. Her initial refraction was RE: -4.50/-1.75x165 6/6 and LE: -4.50/-3x170 6/6.
Despite being compliant with her atropine 0.025% eyedrops nightly, her myopia and AXL still continued to progress in April 2023. Options of increasing her atropine dose versus combination therapy with HAL was discussed and parents opted to add on HAL spectacle lenses on top of her current atropine dose as they were concerned about the potential side effects of near blur and glare associated with higher dose atropine.
Combination treatment with atropine and HAL spectacle lenses proved effective and her myopia stabilized with sustained reversal of AXL elongation noted over a 1-year period.
This graph illustrates the progression and stabilization of myopia in a 6-year-old girl who started on atropine 0.025% nightly in December 2021, later adding HAL spectacle lenses in April 2023. The chart shows a significant reduction in AXL progression over time.
Meet the Authors:
About Dr. Bryan Sim
Dr. Bryan Sim is a Consultant Ophthalmologist with the Myopia Service at the Singapore National Eye Centre (SNEC) with expertise in managing pediatric eye diseases including myopia, neuro-ophthalmic conditions, amblyopia and strabismus. He attained his Ophthalmology Specialist accreditation in 2021, where he was awarded 4 Gold Medals for Best Candidate in Paediatric Ophthalmology; Neuro-Ophthalmology; Oculoplastic & Adnexal Diseases and Generic stations in the Specialists’ Exit Examination. He was subsequently admitted as a fellow of the Royal College of Ophthalmologists (UK) in 2023.
He completed his fellowship in Myopia at the Singapore National Eye Centre (SNEC) in 2023 and strives to provide holistic care and education to the community to alleviate the current Myopia epidemic in Asia and globally. His clinical and research interests focus on myopia control therapies, clinical assessment of myopic optic disc morphology and paediatric Neuro-Ophthalmology. Additionally, he is deeply involved in medical education, serving as co-Course Director of the Myopia Online Course and receiving multiple teaching awards for his contributions to educating medical students, residents, and optometrists.
This content is brought to you thanks to an educational grant from
References
- Ho CL, Wu WF, Liou YM. Dose-Response Relationship of Outdoor Exposure and Myopia Indicators: A Systematic Review and Meta-Analysis of Various Research Methods. Int J Environ Res Public Health. 2019 Jul 21;16(14):2595.
- Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, Fang Y, Pei CL, Wang S, Zhang JZ, Tao LM, Tao FB. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol. 2015 Jul 9;15:73.
- Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012 Feb;119(2):347-54.
- Chia A, Ngo C, Choudry N, Yamakawa Y, Tan D. Atropine Ophthalmic Solution to Reduce Myopia Progression in Pediatric Subjects: The Randomized, Double-Blind Multicenter Phase II APPLE Study. Asia Pac J Ophthalmol (Phila). 2023 Jul-Aug 01;12(4):370-376.
- Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, Tan D. Atropine for the treatment of childhood myopia. Ophthalmology. 2006 Dec;113(12):2285-91.
- Bao J, Huang Y, Li X, Yang A, Zhou F, Wu J, Wang C, Li Y, Lim EW, Spiegel DP, Drobe B, Chen H. Spectacle Lenses With Aspherical Lenslets for Myopia Control vs Single-Vision Spectacle Lenses: A Randomized Clinical Trial. JAMA Ophthalmol. 2022 May 1;140(5):472-478.
- Sankaridurg P, Weng R, Tran H, Spiegel DP, Drobe B, Ha T, Tran YH, Naduvilath T. Spectacle Lenses With Highly Aspherical Lenslets for Slowing Myopia: A Randomized, Double-Blind, Cross-Over Clinical Trial: Parts of these data were presented as a poster at the Annual Research in Vision and Ophthalmology meeting, 2022. Am J Ophthalmol. 2023 Mar;247:18-24.
- Lanca C, Teo A, Vivagandan A, Htoon HM, Najjar RP, Spiegel DP, Pu SH, Saw SM. The Effects of Different Outdoor Environments, Sunglasses and Hats on Light Levels: Implications for Myopia Prevention. Transl Vis Sci Technol. 2019 Jul 18;8(4):7.
- Li X, Huang Y, Yin Z, Liu C, Zhang S, Yang A, Drobe B, Chen H, Bao J. Myopia Control Efficacy of Spectacle Lenses With Aspherical Lenslets: Results of a 3-Year Follow-Up Study. Am J Ophthalmol. 2023 Sep;253:160-168.
- Sankaridurg P, Weng R, Tran H, Spiegel DP, Drobe B, Ha T, Tran YH, Naduvilath T. Spectacle Lenses With Highly Aspherical Lenslets for Slowing Myopia: A Randomized, Double-Blind, Cross-Over Clinical Trial: Parts of these data were presented as a poster at the Annual Research in Vision and Ophthalmology meeting, 2022. Am J Ophthalmol. 2023 Mar;247:18-24.
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.












