Science
GSLS2020 Part 1 - Teens, Treatments and Treatment zones
In this article:
Hello from Las Vegas!! Welcome to the exciting news updates from the Global Specialty Lens Symposium 2020, held January 22-25th. Get ready for a bumper news update! Read on for information on the latest primate research, intervention updates and young adult myopia progression. Jump to the bottom for the link to Update 2: risk-benefit analysis of myopia control, and how to integrate that into practice and inform parents.
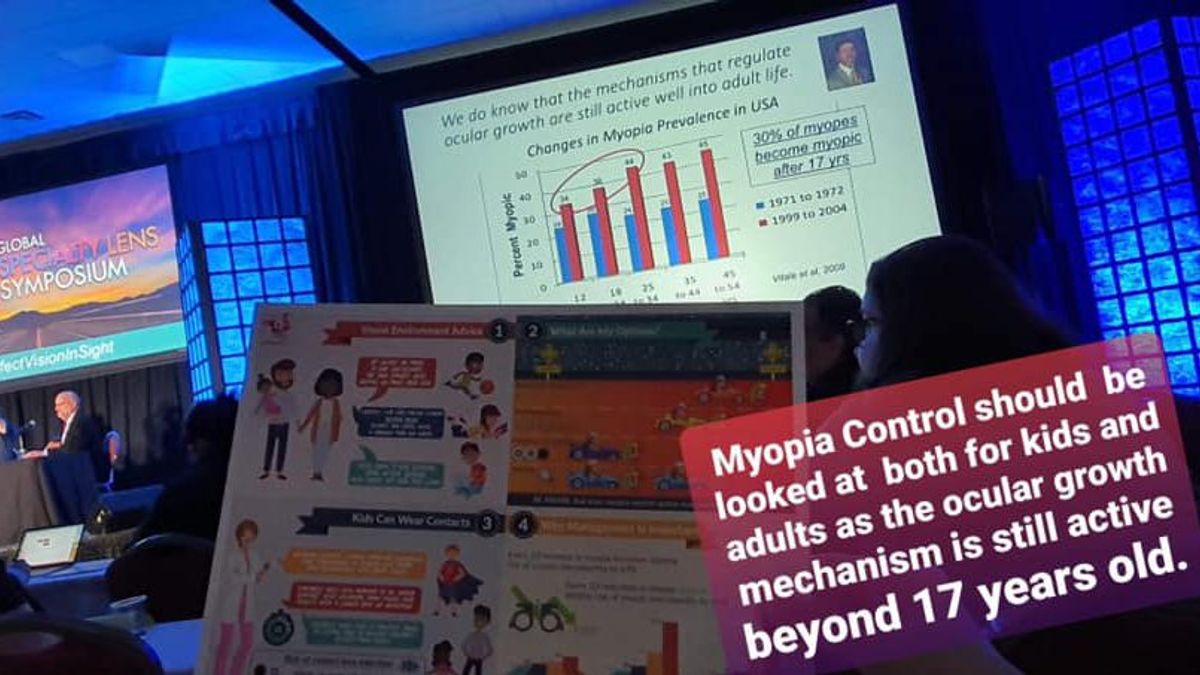
Young Adult Myopia Progression
Big thanks to Jeanette Romualdez, Optometrist from the Phillipines, who composed the above picture and shared it with the Myopia Profile Facebook group. This was from a session which included information on young adult myopia progression.
30% of myopes become myopic after age 17 (that's me - age of onset 19!) so myopia control doesn't conclude when childhood does. Young adult myopia control is a trickier beast though, as:
- We don't have any studies on interventions in this age group
- Side effects of treatments - blur from multifocal contact lenses, specifically designed myopia spectacles or atropine - may be less tolerated, due to lifestyle and visual tasks
- Compliance and safety in contact lens wear can be a bigger challenge in this group.
What are we going to do for them? I believe we need to:
- Consider our optical treatments first. We need to correct myopia as well as control it, so it makes logical sense to firstly choose treatments which do both
- Educate them on the regular eye health management they will require throughout adulthood.
Primate Research and Myopia Mechanisms
Earl Smith (pictured above), from the University of Houston, presented a bunch of fascinating research on what primate research has told us about myopia mechanisms - this time on the crucial concept of simultaneous defocus. It's time to move our thinking from peripheral defocus to simultaneous defocus, where two competing image planes influence eye growth. In practice this means OrthoK, dual focus soft contact lenses and the new DIMS spectacle lens. Here's what we learnt:
- Research where the surface area ratio of the 'add' to distance zones was varied (from 50/50 to around 20/80) showed that any ratio seemed to work better than a single vision lens to modulate eye growth
- The eye DOESN'T appear to average the focal planes; it seems to pay more attention to the myopic plane of defocus, 'an inbuilt safety mechanism' as Earl described it, to manage rampant eye growth. Think of the myopic plane of defocus as the 'add' components of the optical treatment, which are myopically defocused compared to the distance correction portion.
- This dominance of the myopic plane of defocus seems to be an 'all or none' effect, so any 'add' appears to be better than none, BUT
- We're still learning what this treatment threshold might be, both in how much 'add' power is needed and where it needs to land on the retina. This threshold could also vary for the individual based on their inherent optics in combination with the optical treatment, their retinal shape, and also whether they relax their accommodation and 'use the add' at near which influences the optics too, by potentially increasing hyperopic defocus in the system (presumably a bad thing for myopia control). Hence, Earl has advocated as much 'add' as possible in an optical treatment, to maximise the potential simultaneous defocus.
- The periphery is favoured as a site for simultaneous defocus because of the sheer amount of surface area. Earl said that he's been saying 'the periphery' for years and no one has asked him to properly define it yet! So he did another study! Earl showed that the part of the periphery which has a therapeutic effect is not too far out. He presented a study where the 'plus was pushed out' further into the periphery. A 21 degree field (10.5 degrees either side of the fovea, a 2mm central distance optic zone) seemed to have a slightly lesser treatment effect than a 30 degree field (15 degrees either side, a 4mm central optic), although any statistical difference wasn't specified. Larger central optics - more eccentric retinal locations - led to lesser treatment effects. While I'd caution against direct translation to human contact lens optics ("I must have a 4mm optic centre distance lens!") it shows we've still got more to learn about optimum contact lens design.
In summary, our thinking is now moving on from 'peripheral defocus' to 'simultaneous defocus', which helps to picture a more realistic, three dimensional whole-eye effect of these optical treatments rather than just thinking of a two dimensional eye section with a changing image shell.
Interventions for Myopia Control
Jeff Walline (pictured above), from Ohio State University, updated us on interventions for myopia control. So much good stuff!
- OrthoK and soft bifocal / multifocal / dual focus lenses can be considered similar for myopia control efficacy. Both have multiple studies available, although OrthoK has more duration of data available on meta-analysis.
- The new DIMS spectacle lens is super promising and appears to have the strongest results of spectacle lens options. Jeff cautioned that single studies do need replication, though; multiple, independent studies on more of the available interventions are needed.
- Low dose atropine probably needs to be at 0.05% concentration to be effective. Compounding is wildly variable, though, and this is an issue for clinical use in terms of efficacy and side effects. A stable, commercially available preparation could change these recommendations.
- Combination treatments, optical plus low dose atropine, may be helpful, although the evidence is at an early stage. 0.01% has been investigated in these combo studies, with OrthoK or soft multifocal CLs.
- Delaying onset may be the future of myopia control. I've included two slides from Jeff's lecture on this, where 0.025% atropine has been shown to delay onset; outdoor time is the least invasive and most universally applicable treatment to delay onset. The value of delaying onset in terms of final level of myopia is in the top right image.
Click here to read GSLS2020 Part 2: The parents, the patients and your practice
Click here to read GSLS2020 Part 3: Vision lost and vision saved by myopia control
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.