Clinical
Prescribing adds for near esophoria
In this article:
- From a myopia control point of view, esophoria and accommodative lag are the key clinical red flags in assessing your patient’s visual efficiency.
From a myopia control point of view, esophoria and accommodative lag are the key clinical red flags in assessing your patient's visual efficiency, and thankfully both will usually respond positively to a near addition. Studies of progressive spectacle lens prescription for myopia control show a link between faster progression and hence better treatment results in children with esophoria and accommodative lag,1, 2 and myopic children with esophoria specifically selected for bifocal soft lens myopia control have shown strong results.3, 4 In my lectures to colleagues and optometry students, I have espoused a two-system approach to binocular vision assessment, diagnosis and management, which is considering the vergence and accommodation systems ('aiming' and 'focussing', as I describe them to my patients) separately.
Essential reading to explain the below are my notes on how to assess near phoria and it would also be helpful to have read my notes on prescribing adds for accommodative lag. You can also watch my Youtube video on how to measure accommodative lag.
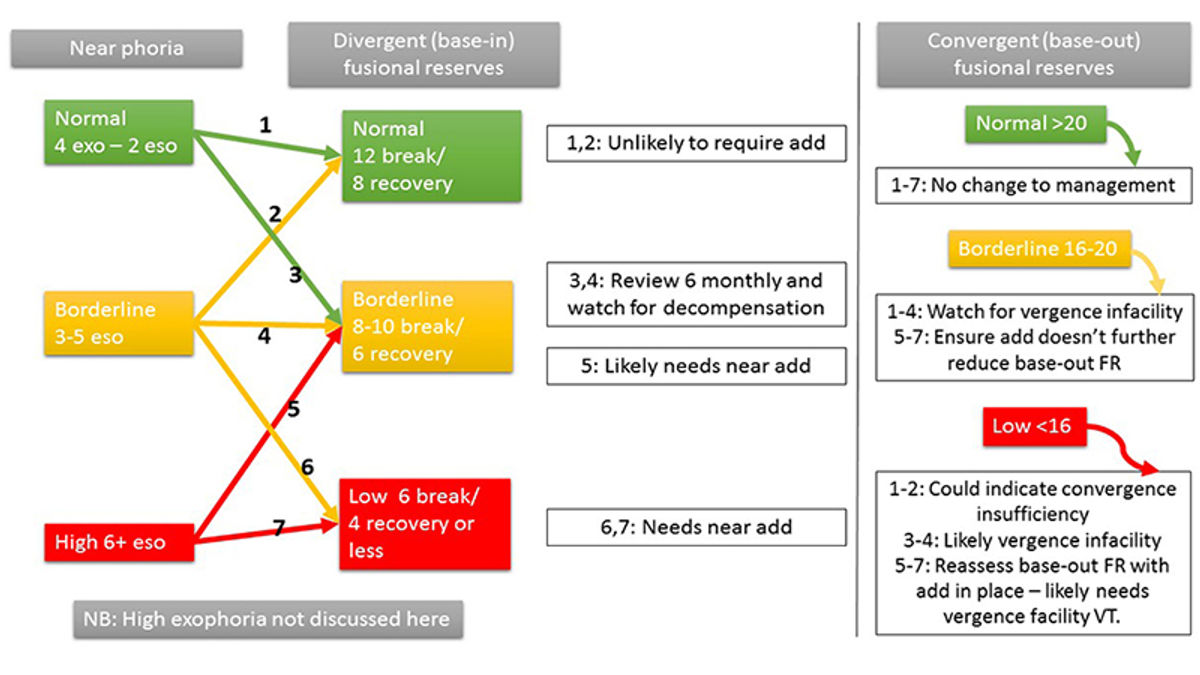
Firstly we've got our phoria result, focussing on the presence of esophoria, and a result for divergent (base-in) fusional reserves at near which describe the stamina, or 'petrol in the tank' to manage the phoria 'posture'. The information below does not delve into management of near exophoria, convergence insufficiency, vergence infacility or distance heterophorias.
If you've determined that your patient needs an add to manage their esophoria, recall that Sheard's criterion describes a compensated (asymptomatic) visual system where the fusional reserves are at least twice the phoria result,5 so ultimately we want to apply as much plus as is needed to achieve this balance. Some general tips:
- Start with an add which is +0.50 less than the near lag of accommodation. Measure the phoria and the divergent (base-in) fusional reserves again and see if Sheard's criterion has been achieved.
- Consider the patient's ability to clear plus, as measured during accommodative facility testing - if they can't clear +2.00 at near, avoid giving them more than this total power in their add.
- Consider also their near working distance - prescribing an add over +1.50 for high school aged children could see them running into trouble looking at a computer screen in bifocal or single vision near spectacles.
If you feel like you've maxed-out the plus and Sheard's criterion is still not being met, then the condition may not be primarily accommodative.6 You can consider the following:
- Adding base-out prism to the add until the phoria / fusional reserves balance is achieved, or at least significantly improved
- Prescribing base-in prism vision training (using a loose prism or prism flippers) to practice repeated divergence tasks at home.
Sometimes, despite your best efforts, you won't be able to reduce the esophoria and/or increase the fusional reserves enough at first prescribing. In almost all of these cases, you'll see a better result after your patient has had some time to adapt and relax into their new add - so use as much plus as you can, and prism also if needed, and assess again after several weeks of wearing time to see if further management with vision training is required.
To delve more into my simplified two-system approach to BV diagnosis and management, you can watch this video entitled Binocular Vision - easier than you think. This one hour lecture includes cases; details easy use of prism correction for vergence disorders; changes to BV in contact lens wear; and why BV matters - for reading and learning in kids, clinical problem solving, and myopia management. You can also download my lecture notes here.
Want to learn more about binocular vision?
Check out my online course Binocular Vision Fundamentals, which starts with my two-system approach to BV assessment and diagnosis. Stepping through understanding of the accommodation and vergence systems, the course then covers clinical tests, diagnostic criteria, prescribing and management. Once this foundation is set, it moves onto clinical communication and the importance of BV in myopia management. Always with a laser sharp focus on the clinical applications.
Included are video examples of assessment techniques and chairside infographic summary downloads to reference in practice.
You can enroll on the first two modules for free, with the full course priced at US$140 if you decide to continue. Reduced course fees by 30% and 50% are available by application for practitioners residing in lower income countries - check out the course page for more information.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
References
- Yang Z, Lan W, Ge J et al. The effectiveness of progressive addition lenses on the progression of myopia in Chinese children. Ophthal Physiol Opt. 2009;29:41-48. (link)
- Gwiazda J, Hyman L, Hussein M et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492-1500. (link)
- Aller TA, Wildsoet C. Bifocal soft contact lenses as a possible myopia control treatment: a case report involving identical twins. Clin Exp Optom. 2008;91:394-399. (link)
- Aller T. Results of a one-year prospective clinical trial (CONTROL) of the use of bifocal soft contact lenses to control myopia progression [abstract]. Ophthal Physiol Opt. 2006:8-9. (link)
- Evans BJW. Detecting binocular vision anomalies in primary eyecare practice. Pickwell's Binocular Vision Anomalies (Fifth Edition). Edinburgh: Butterworth-Heinemann; 2007:12-38. (link)
- Evans BJW. Esophoric conditions. Pickwell's Binocular Vision Anomalies (Fifth Edition). Edinburgh: Butterworth-Heinemann; 2007:109-116. (link)
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.