Clinical
Paradigm Shifts in Understanding Myopia: Asia-Pacific Myopia Management Symposium 2024 Recap #1
Sponsored by
In this article:
Recap #1 of the Asia-Pacific Myopia Management Symposium 2024 discusses new insights on myopia.
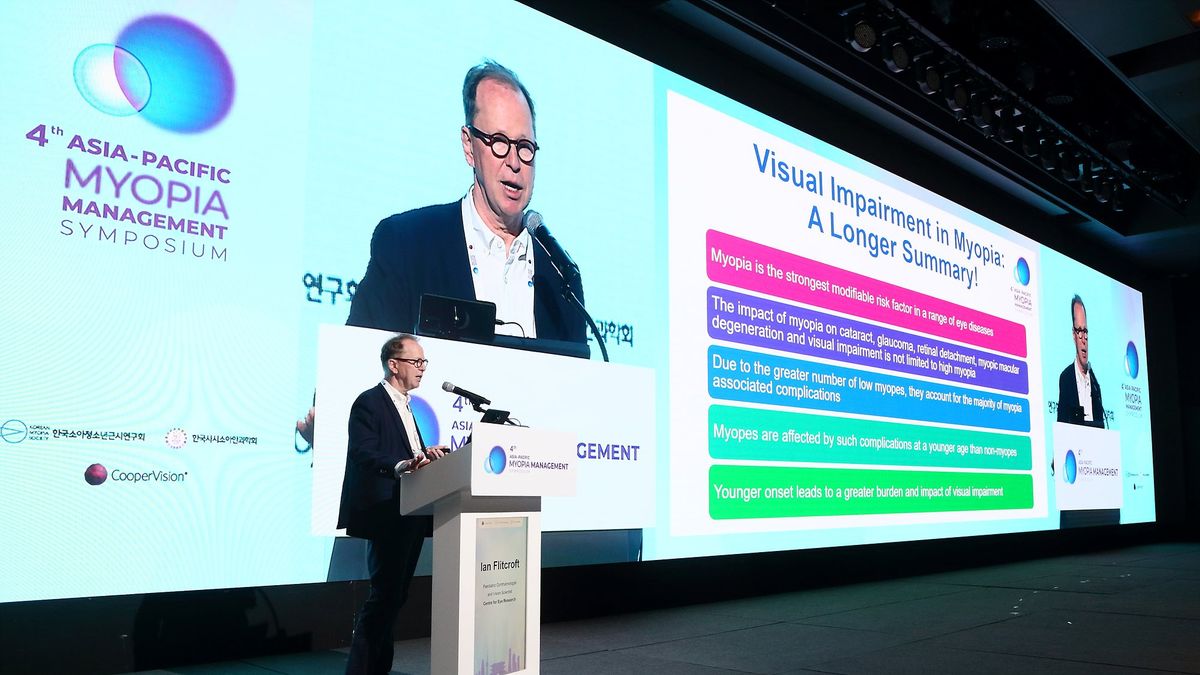
The Asia-Pacific Myopia Management Symposium 2024, held in Seoul, Korea in late October, was championed by CooperVision and brought together global experts to delve into the latest advancements and research in myopia management. Twenty lectures brought out the three key themes of the conference, which were:
- Paradigm Shifts in Understanding Myopia
- Gold Standard in Myopia Interventions (read Recap #2 HERE)
- The Future of Myopia Management (read Recap #3 HERE)
This recap, the first in a series of three, highlights key presentations and discussions that showcased innovative research, clinical approaches, and insights that are reflective of paradigm shifts redefining our understanding of myopia.
Paradigm Shifts in Understanding Myopia
Myopia is increasingly recognized not just as a refractive error but as a serious, lifelong disease with significant health implications. Stories of individuals who have benefitted from early myopia management, such as children whose high myopia risk was mitigated with interventions like MiSight 1-day lenses, illustrate the potential of standardized myopia care to help preserve vision and quality of life. However, myopia management remains far from universal, highlighting the need for it to become standard of care worldwide. Key points emphasized at the symposium were:
- The Seriousness of Myopia: Myopia is increasingly seen as more than a refractive error; it is a significant condition with potentially severe complications. Population data reveals two critical age peaks for rhegmatogenous retinal detachment in Korea: at ages 20-24 and around age 60,1 emphasizing the importance of early intervention to slow progression. These findings highlight that myopia’s risks do not diminish after initial treatment in youth; rather, they persist, requiring ongoing monitoring to prevent and address complications as individuals age. Early intervention is crucial to slow myopia progression in childhood, but sustained care throughout adulthood is equally important to manage risks like retinal detachment, myopic macular degeneration, and glaucoma.
- Broader Health Implications and Myopia’s Image Problem: Myopia is a leading global cause of low vision and blindness when uncorrected, with a high prevalence of uncorrected refractive error among schoolchildren worldwide.2 The ‘high myopia myth’ suggests that "rare complications of common conditions are more common than common complications of rare conditions," highlighting that even low levels of myopia can carry significant health risks. For instance, studies from Singapore reveal that most patients with grade 2 or more myopic macular degeneration are not high myopes.3 Ian Flitcroft (pictured in the cover image above) discussed data showing that low myopia may be more detrimental to eye health than hypertension and smoking are for heart health.4 These insights challenge the notion that only high myopia warrants careful monitoring and intervention, underscoring the need for proactive care and monitoring for all individuals with myopia, regardless of severity.
- Complications in Pathologic Myopia: Pathologic myopia involves extensive structural changes in the posterior segment of the eye, particularly in the retina and sclera. One notable change is staphyloma, a severe “outpouching” of the eye rather than a simple extension of axial elongation, which leads to areas of scleral thinning that reduce its ability to protect nervous tissue.5 This form of myopia can result in complications such as myopic maculopathy, myopic tractional maculopathy, and optic nerve damage, including glaucoma.5 Diagnosing optic nerve damage in myopic patients is challenging due to structural deformities like optic nerve tilting, large peripapillary atrophy (PPA), and myopic macular lesions, which complicate OCT analysis of nerve fibre layers.6 Although treatments are emerging, they remain limited, making prevention essential in managing pathologic myopia effectively.
- Preventing Complications and Emphasizing Early Detection: High myopia substantially increases the risk of retinal detachment. Even with successful surgeries for macula-off retinal detachment, about 61% of patients are left with post-operative vision of 20/50 (6/15) or worse,7,8 reinforcing the importance of prevention. Regular eye exams and comprehensive patient education are essential to managing these risks. Each dioptre of myopia progression adds cumulative risk over time, making it necessary to actively manage even minor progression to reduce long-term impacts on vision health.
A paradigm shift, particularly in how we view low myopia, is crucial for addressing myopia’s broader impact. To make meaningful strides in reducing myopia-related complications worldwide, myopia control must become a standard of care, supported by education and regular examinations. This approach would not only help preserve vision but also improve quality of life for individuals globally, highlighting the importance of integrating myopia management into everyday clinical practice.
What we are still learning
The field of myopia has experienced numerous paradigm shifts, especially with the recognition that myopia can be controlled. However, there remains much to learn about the underlying mechanisms of myopia progression, including why some individuals respond well to certain treatments and others do not. Emerging therapies show promise, such as repeated low-level red-light therapy and AI-based predictive modelling, but their long-term efficacy and integration into clinical practice are still under investigation. This evolving understanding emphasizes that while the field has made significant strides, continued research is essential to refine treatment options, personalize management strategies, and ultimately prevent myopia-related complications across the lifespan.
What this means for practice
In managing myopia, vigilance is essential even at low levels. While low myopia may seem less concerning, it still carries a risk for complications. Early intervention to slow progression is critical to reducing these long-term risks, as even minor increases in myopia can have significant impacts on eye health later in life and add up over time. By proactively managing all myopia, regardless of severity, practitioners can better protect patients from the heightened risks associated with myopic progression, emphasizing prevention and regular monitoring as essential components of comprehensive eye care.
Meet the Authors:
About Jeanne Saw
Jeanne is a clinical optometrist based in Sydney, Australia. She has worked as a research assistant with leading vision scientists, and has a keen interest in myopia control and professional education.
As Manager, Professional Affairs and Partnerships, Jeanne works closely with Dr Kate Gifford in developing content and strategy across Myopia Profile's platforms, and in working with industry partners. Jeanne also writes for the CLINICAL domain of MyopiaProfile.com, and the My Kids Vision website, our public awareness platform.
This content is brought to you thanks to an educational grant from
References
- Park JY, Byun SJ, Woo SJ, Park KH, Park SJ. Increasing trend in rhegmatogenous retinal detachment in Korea from 2004 to 2015. BMC Ophthalmol. 2021 Nov 26;21(1):406.
- Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008 Jan;86(1):63-70.
- Wong YL, Sabanayagam C, Ding Y, Wong CW, Yeo AC, Cheung YB, Cheung G, Chia A, Ohno-Matsui K, Wong TY, Wang JJ, Cheng CY, Hoang QV, Lamoureux E, Saw SM. Prevalence, Risk Factors, and Impact of Myopic Macular Degeneration on Visual Impairment and Functioning Among Adults in Singapore. Invest Ophthalmol Vis Sci. 2018 Sep 4;59(11):4603-4613.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012 Nov;31(6):622-60.
- Ehongo A. Understanding Posterior Staphyloma in Pathologic Myopia: Current Overview, New Input, and Perspectives. Clin Ophthalmol. 2023 Dec 12;17:3825-3853.
- Quiroz-Reyes MA, Quiroz-Gonzalez EA, Quiroz-Gonzalez MA, Lima-Gomez V. Comprehensive assessment of glaucoma in patients with high myopia: a systematic review and meta-analysis with a discussion of structural and functional imaging modalities. Int Ophthalmol. 2024 Oct 11;44(1):405.
- Burton TC, Lambert RW Jr. A predictive model for visual recovery following retinal detachment surgery. Ophthalmology. 1978 Jun;85(6):619-25.
- Tani P, Robertson DM, Langworthy A. Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol. 1981 Nov;92(5):611-20.
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.












