Science
A review of myopic maculopathy classification and treatment
In this article:
Pathological myopia leading to visual impairment is a global concern and has recently been classified for ease of identification and treatment. Further studies investigating current long-term treatment outcomes are needed. However, avoiding development and progression of axial elongation in childhood will reduce the risk of severe myopia-related maculopathy later in life
Paper title: Diagnosis and Treatment of Myopic Maculopathy
Authors: Yokoi, Tae (1), Ohno-Matsui, Kyoko (1)
- Department of Ophthalmology and Visual Science, Tokyo Medical and Dental University, Tokyo, Japan.
Date: Dec 2018
Reference: Yokoi T, Ohno-Matsui K. Diagnosis and Treatment of Myopic Maculopathy. Asia Pac J Ophthalmol (Phila). 2018 Nov-Dec;7(6):415-421
Summary
Myopic maculopathy (MM) is a major cause of global visual impairment, with high degrees of myopia being associated with more pronounced visual loss. However, due to varying types and severity of maculopathy there have been no standardised definitions to allow for further studies into prevalence or clinical analysis of sub-types. This review article described a system suggested by the Meta-Analysis for Pathological Myopia (META-PM) Study group (2015) to classify MM and define the stage where pathological myopia can be said to be present.1
Five categories of myopic maculopathy lesions were defined based on long-term clinical observations of progression patterns and the risk of myopic choroidal neovascularisation (myopic CNV) at each stage:
- Category 0: no myopic retinal lesions
- Category 1: tessellated fundus only
- Category 2: diffuse chorio-retinal atrophy
- Category 3: patchy chorio-retinal atrophy (or macular Bruch membrane rupture)
- Category 4: macular atrophy
Three additional ‘plus’ signs were included in the classification due to their association with central vision loss and can be present in any of the MM categories:
- Lacquer cracks (considered a precursor to myopic CNV which increase in width and number over time),
- Myopic CNV and
- Fuch’s spots (pigmented cells which proliferate myopic CNV giving rise to Fuch’s spot which may further advance to CNV-related macular atrophy).
Using the META-PM classification system, pathological myopia can be defined as MM from category 2 or above, in the presence of a ‘plus’ sign or posterior staphyloma. The review included details of each MM category. Visual loss, ocular axial elongation and area size of atrophy increase with the category levels. Patchy chorio-retinal atrophy is accompanied by a reduction in the retinal pigment epithelium and choroid layer thickness. It usually spares central vision until end-stage myopic chorio-retinal atrophy where there is fusion of patchy atrophy.
The authors analysed a longitudinal study which found that adults with pathological myopia had been recorded as having longer axial lengths and signs of peripapillary diffuse choroidal atrophy (PDCA) as children. The study suggested that PDCA in children can be taken as an indicator of pathological myopia later in life and if diffuse atrophy around the optic disc is apparent in childhood, that preventative steps are required to avoid axial elongation.2
The authors also discussed the use of Optical Coherence Tomography (OCT), fluorescein angiography (FA) and indocyanine green angiography (ICGA) for detecting and analysing the presence of CNV-related macular atrophy. Although OCT and FA were able to detect most changes in the retinal layers although lacquer cracks were found to be more difficult to detect using OCT, unless particularly large.
First-line treatment for myopia CNV is currently anti-vascular endothelial growth factor (anti-VEGF). However, some studies have shown that despite good initial best corrected visual acuity (BCVA) the improvement may not last long-term, possibly correlating with repeated treatments.
What does this mean for my practice?
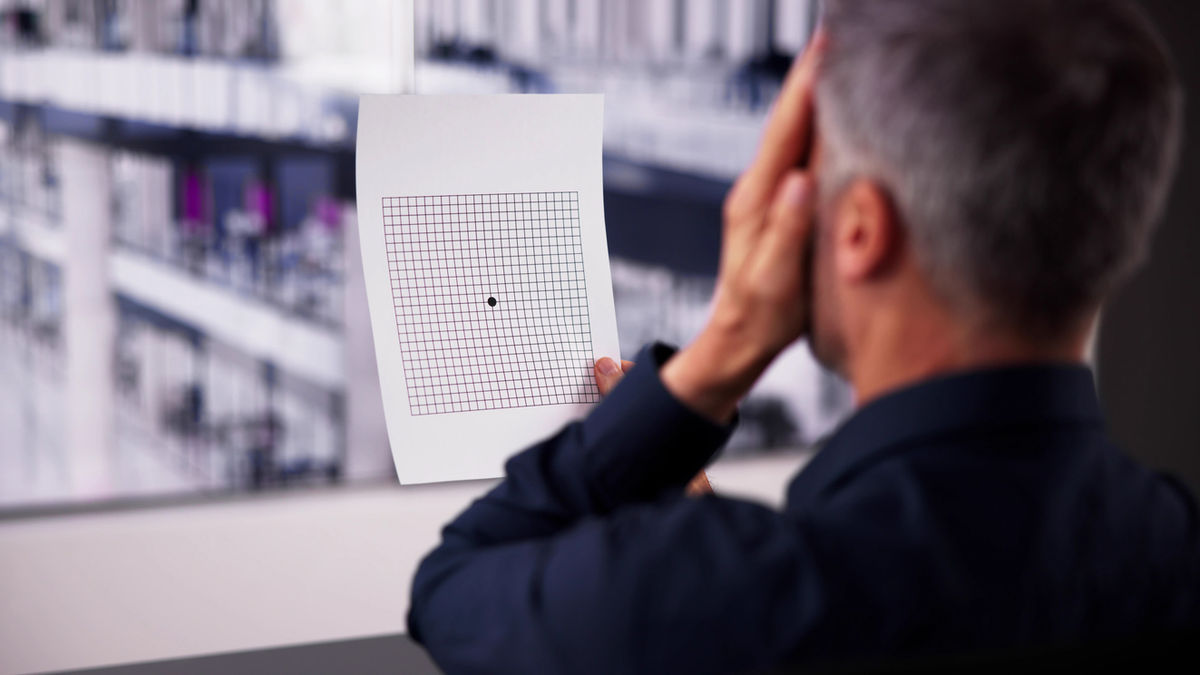
Although not every highly myopic eye will develop potentially sight-threatening myopia related CNV, peripapillary diffuse atrophy in childhood may suggest advanced myopic chorio-retinal atrophy in adulthood and as such, highly myopic children showing atrophic development around the optic disc should be investigated further.
Treatment can be planned according to OCT and FA findings and although anti-VEGF treatment is available, the benefits may not be long-lasting.
Preventing myopia and high myopia from developing childhood would limit axial elongation and therefore reduce the risks of macular complications in later life.
What do we still need to learn?
Anti-VEGF intravitreal injection therapies similar to those used to treat AMD have provided a safe treatment option for myopic CNV, improving visual acuity. However, repeated intravitreal injections have also been shown to have adverse effects and visual acuity can decrease.3
Further studies are needed to assess the optimal frequency and long-term outcomes of Anti-VEGF therapy in myopic CNV.
Abstract
Title: Diagnosis and treatment of myopic maculopathy
Authors: Tae Yokoi, Kyoko Ohno-Matsui
Purpose: Visual impairment resulting from pathological myopia is a serious issue worldwide. This is mainly due to the development of different types of myopia maculopathy. Despite being a major cause of visual impairment worldwide, myopic maculopathy was not consistently defined
Methods: To overcome this problem, in 2015 the Meta-Analysis for Pathologic Myopia Study Group proposed a simplified, uniform classification system for myopic maculopathy. Among several lesions of myopic maculopathy, myopic choroidal neovascularization (CNV) is one of the most common and severe vision-threatening complications. Recent large clinical trials have reported a good initial efficacy for visual acuity improvement by application of anti-vascular endothelial growth factor therapy for myopic CNVs. However, long-term clinical studies demonstrate a gradual decrease in the visual acuity gain and return to the baseline level due to the development of myopic CNV-related macular atrophy.
Results: Regarding visual impairment caused by advanced myopic chorioretinal atrophy, the only way to prevent blindness is to prevent myopia from developing or progressing at a young age before the axial length elongates extremely.
Conclusions: As peripapillary diffuse atrophy in childhood may be an indicator of more advanced myopic chorioretinal atrophy in later life, some preventive measures should be considered in such children.
Meet the Authors:
About Ailsa Lane
Ailsa Lane is a contact lens optician based in Kent, England. She is currently completing her Advanced Diploma In Contact Lens Practice with Honours, which has ignited her interest and skills in understanding scientific research and finding its translations to clinical practice.
Read Ailsa's work in the SCIENCE domain of MyopiaProfile.com.
References
- Ohno-Matsui K, Kawasaki R, Jonas JB, Cheung CM, Saw SM, Verhoeven VJ, Klaver CC, Moriyama M, Shinohara K, Kawasaki Y, Yamazaki M, Meuer S, Ishibashi T, Yasuda M, Yamashita H, Sugano A, Wang JJ, Mitchell P, Wong TY; META-analysis for Pathologic Myopia (META-PM) Study Group. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015 May;159(5):877-83.e7 [Link to abstract]
- Yokoi T, Jonas JB, Shimada N, Nagaoka N, Moriyama M, Yoshida T, Ohno-Matsui K. Peripapillary Diffuse Chorioretinal Atrophy in Children as a Sign of Eventual Pathologic Myopia in Adults. Ophthalmology. 2016 Aug;123(8):1783-1787 [Link to abstract]
- Onishi Y, Yokoi T, Kasahara K, Yoshida T, Nagaoka N, Shinohara K, Kaneko Y, Suga M, Uramoto K, Ohno-Tanaka A, Ohno-Matsui K. FIVE-YEAR OUTCOMES OF INTRAVITREAL RANIBIZUMAB FOR CHOROIDAL NEOVASCULARIZATION IN PATIENTS WITH PATHOLOGIC MYOPIA. Retina. 2019 Jul;39(7):1289-1298 [Link to abstract]
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.










