Science
The effect of orthokeratology on ocular aberrations
In this article:
This article delves into the research literature to provide an overview of changes to ocular aberrations that are induced from orthokeratology (OK) lens wear, towards providing a background for understanding potential influence of OK induced changes to ocular aberrations on slowing progression of myopia.
Early research
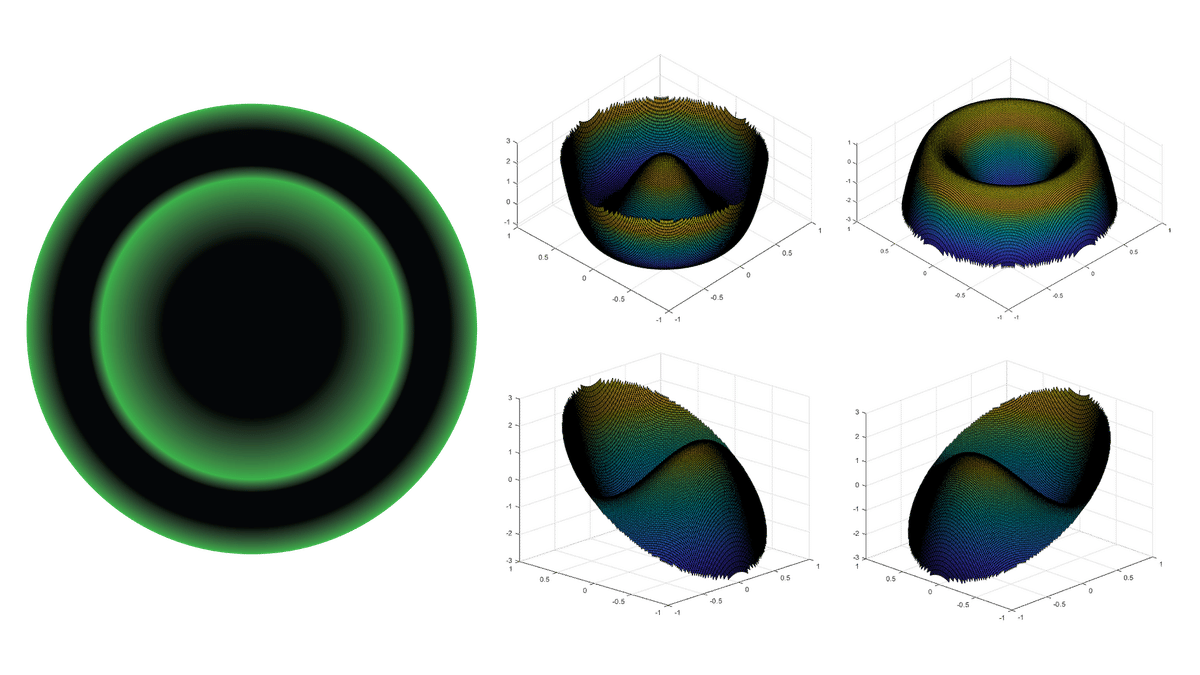
The earliest published research on changes to wavefront aberrations was calculated from change to corneal topography over 3 months of wearing Emerald lenses. Wavefront aberrations calculated from the anterior cornea are not the same as whole eye aberrations, however OK imparts its refractive effect to the anterior cornea so it's reasonable to expect changes to corneal surface derived wavefront aberrations to align reasonably well with changes to measured whole eye aberrations - more on this below.
In this research, which was published in two journals, third order aberrations were found to increase by 0.053µm for 3mm pupils and 0.31µm for 6mm pupils(1,2). Vertical coma (Z7) and horizontal coma (Z8) fall within the third order and were found to change by -0.026µm(Z7), 0.051µm(Z8) for 3mm pupils and by -0.246µm(Z7), 0.345µm(Z8) for 6mm pupils. Fourth order aberrations, which contain spherical aberration increased by 0.042µm for 3mm pupils and 0.552µm for 6mm pupils, however the individual spherical aberration component wasn't analysed. The authors concluded that corneal higher order aberrations increased even in clinically successful cases and that the magnitude of higher order aberrations correlated with the degree of myopia correction.
The same authors later reported changes to whole eye aberrations measured across a 4mm pupil to find 0.185µm increase to third order aberrations and 0.096µm increase to fourth order aberrations. In this research they also measured change to contrast sensitivity function (CSF) using CSV-1000 charts (Vector Vision Co) to reveal that increasing ocular aberrations were correlated with both increase to myopia correction from OK and reduction to CSF(3). A similar negative correlation between change to CSF measured using a different instrument (Mesotest II, Oculus) and higher order aberrations was subsequently reported by the same authors(4). This degradation to CSF adding further weight to the concerns they raised from their previous research that large myopic reduction by OK should be avoided so as to not decrease optical quality(2).
Spherical aberration
In short term wear of up to 1 hour, SA is reported to increase by 0.027µm (4.5mm pupil) after 15mins, 0.028µm after 30mins and 0.044µm after 60mins of OK lens wear(5).
Over the longer term, SA derived from whole eye aberrometry was found to change by 0.357µm (6.5mm pupil) after the first night of OK and a greater change of 0.717µm after eight nights of wear with no further change, indicating stability, for the rest of the year(6). A similar timescale but over shorter total study duration was reported by Lian et al(7) where SA changed by 0.23µm (6mm pupil) after the first night wear with a greater change of 0.4µm at 1 week and no further change by 1 month.
When it comes to regression of effect during the day after 6 months of OK lens wear, change to SA induced by OK was found to reduce during the morning by 0.072µm (6.5mm pupil) and during the afternoon by 0.042µm(9).
Coma
In short term wear of up to 1 hour, combined coma (Z7+Z8) is reported to increase by 0.035µm after 15mins, 0.068µm after 30mins and 0.084µm after 60mins of OK lens wear measured across a 4.5mm pupil(5).
Over the longer term, change to combined coma (Z7+Z8) was found to change by 0.151µm (6.5mm pupil) after the first night of OK and a greater change of 0.288µm after eight nights of wear reaching the highest change of 0.423µm after 3 months of lens wear(6). Thereafter coma reduced to lower levels of change for the remainder of the year during which measurements were taken. Lian et al(7) instead reported 0.16µm (6mm pupil) change to coma after the first night of OK lens wear with similar amounts of coma measured after 1 week and 1 month of OK lens wear.
Coma is essentially created by the OK induced treatment zone (TZ) decentering, with greater amounts of decentration correlating with increasing coma (8). This offers a possible explanation for the disagreement between the studies reporting long term OK induced changes to coma in that any variability across day to day lens wear characteristics could potentially alter TZ decentration and thereby influence measured coma.
Whereas SA was found to reduce during the day without lenses (see above), change in combined coma (Z7+Z8) induced by 6 months of overnight OK lens wear failed to reveal significant regression of effect during the day (8am 0.428µm vs 6pm 0.371µm)(9).
Whole eye vs cornea derived wavefront aberrations
While I earlier stated that OK induced changes to wavefront aberrations derived from corneal topography should be similar to whole eye aberration measurements, two studies have reported on data obtained from instruments that simultaneously capture corneal topography and whole eye aberrations to find that this isn't quite the case.
Gifford et at (10) found changes to SA derived from corneal topography to be slightly higher than measured by whole eye aberrometry after the first night of lens wear (cornea 0.084µm, whole eye 0.059µm, both 5mm pupil) and first week of lens wear (cornea 0.155µm, whole eye 0.099µm). The increase in SA from 1 night to 1 week of wear matches reports from other research, however the authors reported an interesting observation that there was significantly greater increase to corneal aberrations than whole eye aberrations between these two visits, leading them to suggest a possible ocular compensation effect over time to OK induced changes to corneal SA. The opposite was found for combined coma where change in response to OK lens wear was found to instead be higher in whole eye wavefront measurements (First night: cornea 0.01µm, whole eye 0.055µm; 1 week: cornea 0.094µm, whole eye 0.135µm). Unlike SA, for coma the increase in coma from the first night to 1 week of wear was similar for corneal and whole eye wavefront aberrations indicating no evidence of a potential compensation effect for coma.
Chen et al (11) instead found change to whole eye SA after 1 month of OK lens wear to be slightly higher than wavefront aberrations derived from corneal topography (cornea 0.11µm, whole eye 0.14µm, 4mm pupil). They found that change to corneal derived vertical coma (Z7) was higher than for the whole eye (cornea 0.08µm vs whole eye 0.01µm). Horizontal coma (Z8), however, changed by a greater but similar amount between cornea and whole eye measurements (cornea 0.2µm vs whole eye 0.21µm). The differential of change to corneal vs whole eye coma between vertical and horizontal coma led the authors to suggest a possible ocular response compensation to vertical coma where the vertical coma induced by OK was being balanced by change to internal eye aberrations.
Effect on wavefront aberrations from discontinuing OK lens wear
The increase to third and fourth order ocular aberrations measured after 1 year of wear was found to return to baseline levels within 1 week of discontinuing OK lens wear(12).
Summary
The combined research to date reveals that change to cornea topography derived wavefront aberrations are associated with the degree of refractive change provided by OK lenses, which is not a surprise given that any change to corneal topography profile will have an effect on corneal topography derived wavefront aberrations. Correlation between the amount of refractive change induced by OK lens wear and measured whole eye aberrations is also reported, which is again not a surprise given that OK has been shown to provide it's refractive effect principally from change in curvature to the anterior corneal surface (13). Any changes to the cornea, which forms the major refractive surface of the eye, will as a consequence influence measured whole eye aberrations.
However, when measured simultaneously, there are subtle differences between changes to corneal derived higher order aberrations and whole eye higher order aberrations in response to OK lens wear are reported, indicating either limitations to measurement accuracy or that other refractive surfaces beyond the anterior cornea are being affected by OK lens wear. This has led to suggestions of possibility for internal eye response to OK induced SA(10) and vertical coma(11).
OK induced changes to wavefront aberrations increase progressively in the first week of overnight lens wear, though there is disagreement on whether changes to coma stabilise after the first night of wear (8) or takes up to 3 months to become stable (7). Any OK lens induced changes to wavefront aberrations reduce to baseline values within 1 week of discontinuation of lens wear.
The reported OK induced changes to wavefront aberrations raise obvious questions on whether they could be influential in providing the myopia controlling effect that OK has been shown to provide.
Further reading in our science series on aberrations
Meet the Authors:
About Paul Gifford
Dr Paul Gifford is an eyecare industry innovator drawing on experience that includes every facet of optometry clinical practice, transitioning to research and academia with a PhD in ortho-k and contact lens optics, and now working full time on Myopia Profile, the world-leading educational platform that he co-founded with Dr Kate Gifford. Paul is an Adjunct Senior Lecturer at UNSW, Australia, and Visiting Associate Professor at University of Waterloo, Canada. He holds three professional fellowships, more than 50 peer reviewed and professional publications, has been conferred several prestigious research awards and grants, and has presented more than 60 conference lectures.
References
- Hiraoka T, Matsumoto Y, Okamoto F, Yamaguchi T, Hirohara Y, Mihashi T, Oshika T. Corneal higher-order aberrations induced by overnight orthokeratology. Am J Ophthalmol. 2005;139:429-46 (link)
- Hiraoka T, Okamoto F, Kaji Y, Oshika T. Optical quality of the cornea after overnight orthokeratology. Cornea. 2006;25:S59-63 (link)
- Hiraoka T, Okamoto C, Ishii Y, Kakita T, Oshika T. Contrast sensitivity function and ocular higher-order aberrations following overnight orthokeratology. Invest Ophthalmol Vis Sci. 2007;48:550-6 (link)
- Hiraoka T, Okamoto C, Ishii Y, Takahira T, Kakita T, Oshika T. Mesopic contrast sensitivity and ocular higher-order aberrations after overnight orthokeratology. Am J Ophthalmol 2008;145:645-55 (link)
- Lu F, Simpson T, Sorbara L, Fonn D. Malleability of the ocular surface in response to mechanical tress induced by orthokeratology contact lenses. Cornea 2008;27:133-141 (link)
- Stillitano I, Schor P, Lipener C, Hofling-Lima AL. Long-term follow-up of orthokeratology corneal reshaping using wavefront aberrometry and contrast sensitivity. Eye & Contact Lens. 2008;34:140-5 (link)
- Lian Y, Shen M, Huang S, Yuan Y, Wang Y, Zhu D, Jiang J, Mao X, Wang J, Lu F. Corneal reshaping and wavefront aberrations during overnight orthokeratology. Eye and Contact Lens. 2014;40:161-8 (link)
- Hiraoka T, Mihashi T, Okamoto C, Okamoto F, Hirohara Y, Oshika T. Influence of induced decentered orthokeratology lens on ocular higher order wavefront aberrations and contrast sensitivity function. J Cataract Refract Surg. 2009;35:1918-26 (link)
- Stillitano I, Schor P, Lipener C, Hofling-Lima AL. Stability of wavefront aberrations during the daytime after 6 months of overnight orthokeratology corneal reshaping. J Refract Surg. 2007;23:978-983 (link)
- Gifford P, Li M, Lu H, Panjaya M, Swarbrick HA. Corneal versus ocular aberrations after overnight orthokeratology. Optom Vis Sci. 2013;90:439-447 (link)
- Chen Q, Li M, Yuan Y, Me R, Yu Y, Shi G, Ke B. Interaction between corneal and ocular aberrations induced by orthokeratology and its influential factors. Bio Med Res Int. 2017;Article ID 3703854 (link)
- Hiraoka T, Okamoto C, Ishii Y, Okamoto F, Oshika T. Recovery of corneal irregular astigmatism, ocular higher-order aberrations, and contrast sensitivity after discontinuation of overnight orthokeratology. Br J Ophthalmol. 2009;93:203-208 (link)
- Swarbrick HA, Wong G, O'Leary DJ. Corneal response to orthokeratology. Optom Vis Sci. 1998 Nov;75(11):791-9 (link)
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.










