Clinical
What about the exophores?
In this article:
While esophoria and myopia have a long-associated link,1-3 exophoria must also be on our myopia management agenda. The punchline, up front - research has shown that of kids with intermittent exotropia, 50% are myopic by age 10 and 90% are myopic by age 20,4 and we need to be extra wary if considering fitting a myopic child like this into contact lenses.
Our first consideration in myopia management is correcting the ametropia with spectacles or contact lenses - while contact lens options have generally shown the strongest myopia control efficacy of optical treatments,5 sometimes spectacles may be the better choice. This generally occurs when contact lens correction will not provide adequate sole management of BV disorders - a key example being the child exhibiting a large exophoria or intermittent exotropia in spectacles.
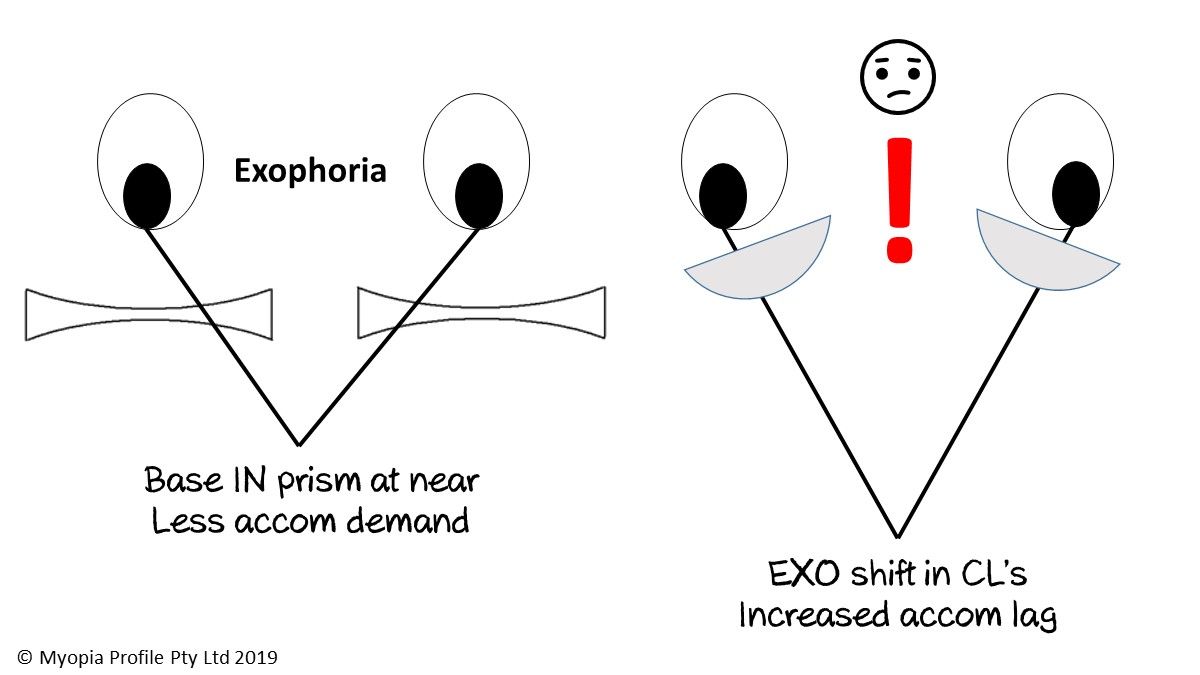
As described in Specs to Contact Lenses - What happens to BV?, and seen in the image above, changing a myope from spectacle to contact lens wear can alter their BV function. The myope reading through their spectacles experiences base-in prism at near, moving the image further away. Looking away from the optical centre of the lens also reduces the power, effectively reducing the accommodative demand. When this myope changes to a single vision distance (SVD) contact lens, they must increase their accommodative effort, and they will also show an exophoric shift as they lose the base-in spectacle correction and have to converge more by themselves.6
If a child or young adult is exophoric in their spectacles, this will likely increase in contact lens correction and could lead to decompensation of the phoria or increasing frequency of the intermittent tropia.
Ajay's story
Ajay was referred for orthokeratology (OK) fitting at age 11. At age 10 his spectacle refraction was R-2.00/-0.75x90 and L -2.50/-1.25x90. He was referred after his refractive progression in one year was R -0.75DS and L -2.50DS. On examination, I noted that Ajay exhibited a left eye almost-constant convergence insufficiency exotropia (worse at near than at distance). Intermittent exotropia (IXT) has been shown to lead to a higher prevalence of myopia than in the general population, with one study showing that over a mean follow up period of 8 years, almost 50% of children with IXT had developed myopia by age 10, and over 90% had developed myopia by age 20. Interestingly, undergoing surgery for IXT between 6-15 years of age had no significant effect on the rate of myopia progression.4
It is unknown whether myopia development or progression could trigger IXT, or whether the reverse is true. If myopia comes first, perhaps the decreased demand for accommodation results in lower convergence and for those predisposed, decompensation into significant exophoria or tropia. If the IXT comes first, perhaps it requires increased accommodative effort to drive accurate near point focus, leading to possible pseudo-myopia at distance. Similarly, disrupted fusion from anisomyopia in early childhood can lead to exotropia, with the reverse also being true - that suppression from exotropia can cause sensory strabismus and a type of form deprivation myopia.7
Shifting from spectacles to LASIK correction in young adults has also been associated with exophoric and tropic shifts.8 Similarly for Ajay, shifting from a spectacle correction where an IXT which was nearly constant could lead to decompensation into a constant exotropia. Despite being referred for OK fitting, Ajay's BV made him an unsuitable candidate, so Ajay has stayed in spectacle correction for the year since, with both prism correction for fusion and vision training provided to improve his binocularity. While a -0.50 shift in both R&L eyes has occurred over this subsequent year, this is much less than the year prior and while the sensory component of Ajay's strabismus has improved, in time he may be suitable to be fit with OK or another soft myopia controlling contact lens.
Mary's story
Mary had unfortunately progressed to a high aniso-myopic prescription by the time I first saw her at age 11, and had a similar BV picture to Ajay - left IXT. Mary's IXT was not as severe as Ajay's, though, and she was very motivated to wear contact lenses, so she was initially fit with OrthoK. Full correction was achieved in her right eye and a -1.75DS residual occurred in her L eye. I was happy enough with this option for her, given the HM-PRO study showed that partial correction of high myopia has been shown to have a similar myopia controlling effect to full correction,9 and she still needed over-specs with base-in prism to improve consistency of her fusion.
After a year in this correction, Mary's right eye was refractively stable but her left eye had progressed by -1.50DS. A terrible outcome! What has occurred? Mary's is a case where an 'ideal' correction turned out to be not-so-ideal due to complicating factors. Firstly, having a full OK correction in her right eye was a disincentive to wear the over-specs, so her left eye frequently suffered undercorrection, which has been shown to increase myopia progression.10 Secondly, wearing the over-specs infrequently meant less consistency of binocular fusion, so the poor left eye suffered a double whammy of undercorrection and intermittent suppression.
Mary was discontinued from OrthoK and fit into full correction, distance centred toric multifocal soft contact lenses with a +2.50 Add. On first review, she returned with complaints of blur and 6/7.5- (20/25-) monocular acuity, despite an over-retinoscopy result of R&L plano. I didn't think she needed additional minus - instead she was prescribed a +2.00 Add and has worn these successfully for over a year now, with refractive stability achieved. This management pathway is in alignment with the suggestion of the first researcher to publish a randomized controlled trial on multifocal contact lens myopia control - Dr Jeff Walline. You can read more in his blog entitled Vision with Pediatric Bifocal Wear. Mary has been working hard on vision training to improve her binocular stability and base-out (convergent) fusional reserves with loose prism, with the understanding that she needs to continue showing reduction in the IXT to stay in her contact lenses.
So in conclusion - beware the exophore in myopic contact lens fitting! Read more in Four reasons why binocular vision matters in myopia management, and about how great contact lenses are for esophores in The esophoric myopia and contact lenses. If you want to understand a bit more about how I factor BV into a myopia management strategy, check out our Clinical Decision Trees and on putting it into practice, our Clinical Management Infographic.
Want to learn more about binocular vision?
Check out my online course Binocular Vision Fundamentals, which starts with my two-system approach to BV assessment and diagnosis. Stepping through understanding of the accommodation and vergence systems, the course then covers clinical tests, diagnostic criteria, prescribing and management. Once this foundation is set, it moves onto clinical communication and the importance of BV in myopia management. Always with a laser sharp focus on the clinical applications.
Included are video examples of assessment techniques and chairside infographic summary downloads to reference in practice.
You can enroll on the first two modules for free, with the full course priced at US$140 if you decide to continue. Reduced course fees by 30% and 50% are available by application for practitioners residing in lower income countries - check out the course page for more information.
Meet the Authors:
About Kate Gifford
Dr Kate Gifford is an internationally renowned clinician-scientist optometrist and peer educator, and a Visiting Research Fellow at Queensland University of Technology, Brisbane, Australia. She holds a PhD in contact lens optics in myopia, four professional fellowships, over 100 peer reviewed and professional publications, and has presented more than 200 conference lectures. Kate is the Chair of the Clinical Management Guidelines Committee of the International Myopia Institute. In 2016 Kate co-founded Myopia Profile with Dr Paul Gifford; the world-leading educational platform on childhood myopia management. After 13 years of clinical practice ownership, Kate now works full time on Myopia Profile.
References
- Gwiazda J, Grice K, Thorn F. Response AC/A ratios are elevated in myopic children. Ophthalmic Physiol Opt. 1999;19:173-179. (link)
- Yang Z, Lan W, Ge J, Liu W, Chen X, Chen L, Yu M. The effectiveness of progressive addition lenses on the progression of myopia in Chinese children. Ophthal Physiol Opt. 2009;29:41-48. (link)
- Drobe B, de Saint-André R. The pre-myopic syndrome. Ophthal Physiol Opt. 1995;15:375-378. (link)
- Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. The development of myopia among children with intermittent exotropia. Am J Ophthalmol. 2010;149:503-507. (link)
- Huang J, Wen D, Wang Q, et al. Efficacy Comparison of 16 Interventions for Myopia Control in Children: A Network Meta-analysis. Ophthalmol. 2016;123:697-708. (link)
- Hunt OA, Wolffsohn JS, Garcia-Resua C. Ocular motor triad with single vision contact lenses compared to spectacle lenses. Cont Lens Anterior Eye. 2006;29:239-245. (link)
- Kekunnaya R, Chandrasekharan A, Sachdeva V. Management of Strabismus in Myopes. Middle East Afr J Ophthalmol. 2015;22:298-306. (link)
- Kowal L, Battu R, Kushner B. Refractive surgery and strabismus. Clin Exp Ophthalmol. 2005;33:90-96. (link)
- Charm J, Cho P. High myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90:530-539. (link)
- Chung K, Mohidin N, O'Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Research. 2002;42:2555-2559. (link)
Enormous thanks to our visionary sponsors
Myopia Profile’s growth into a world leading platform has been made possible through the support of our visionary sponsors, who share our mission to improve children’s vision care worldwide. Click on their logos to learn about how these companies are innovating and developing resources with us to support you in managing your patients with myopia.










